Chronic Obstructive Pulmonary Diseases (COPD)
- Chronic obstructive pulmonary disease is a disease state characterized by the presence of airflow obstruction due to chronic bronchitis and emphysema; the airflow obstruction is generally progressive may be partially reversible and may be accompanied by airway hyperactivity.
- COPD or chronic obstructive pulmonary disease, is a progressive disease that makes it hard to breath.progressives means the disease gets worse over time"
- Chronic Obstructive Pulmonary Disease (COPD) makes it hard for you to breath. Coughing up mucus is often the first sigh of COPD .Chronic bronchitis and emphysema are common COPDs.
- The airway obstruction means FEV1 <80% predicted and FEV1/VC ratio <70% which does not changed markedly over several months.
- COPD can cause coughing that produces large amount of mucus(a slimy substances),
- Wheezing
- Shortness of breath
- Chest tightness
- Productive cough and other symptoms
- Cigarette smoking is the leading cause of COPD. Most people who have COPD smoke or use to smoke.
- COPD is typically worsens over time, primary sympotoms include: shortness of breath,cough and sputum production
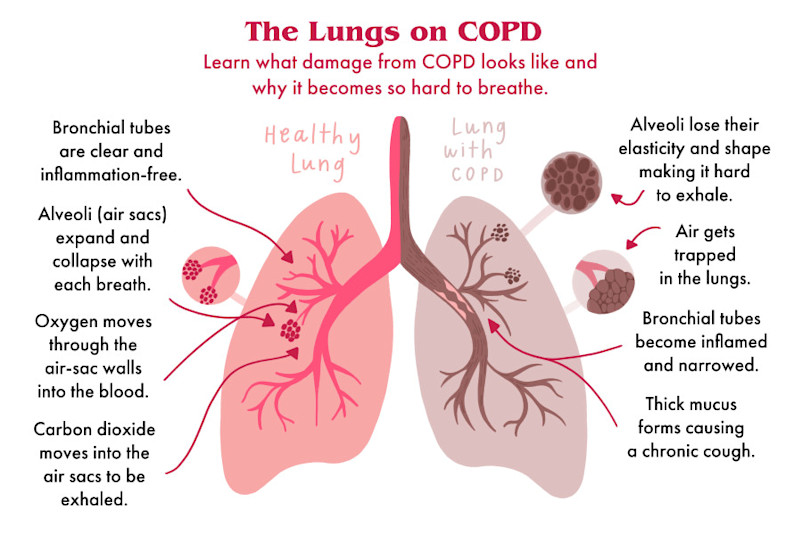
- In COPD, less air flows in and out of the airways because of one or more of the following:
- The airways and air sacs lose their elastic quality.
- The walls between many of the air sacs are destroyed.
- The walls of the airways become thick and inflamed
- The airways make more mucus the usual, which can clog them.
Why is emphysema considered to be an obstructive airways disease? Is there any mechanical obstruction?
Because emphysema affects the peripheral airways ,is is not anatomically specking, an obstructive disease, and there is no mechanical obstruction. However, it is functionally an Obstructive disease,because destruction of the septal walls prevents the elastic recoil that is necessary to push air out of the lungs. Thus, in effect, there is limitation of airflow, just as there would be if there were mechanical obstruction
Classification and diagnosis of chronic obstructive pulmonary disease
Severity Spirometry Symptoms
1.Mild FEV1 (60-79%) Smoker's cough +- exertional dyspnoea
2. Moderate FEV1 (40-59%) Exertion dyspnoea +- wheeze,Cough +- sputum
3. Severe FEV1 <40% predication Breathlessness, wheeze and prominent cough, swelling
legs( features of heart failure)
2. Moderate FEV1 (40-59%) Exertion dyspnoea +- wheeze,Cough +- sputum
3. Severe FEV1 <40% predication Breathlessness, wheeze and prominent cough, swelling
legs( features of heart failure)
Predisposing Factors of Chornic obstructive Pulmonary disease
- Smoking
- Enviromental pollution ( dust, smoke etc)
- Respiratory tract infection
- Alpha1-antitrypsin deficeiency
- Occupation exposure (fumes)
- Exposure to dampness,fog etc
- sudden change in temperature
Precipating factors of acute exacerbation of COPD
- Respiratorytract infection
- Pneumothorax
- Use os sedative drugs
- Left venttricular failure
- Pulmonary embolism
Clinical feature of Chronic Obstructive Pulmonary disease
- Symptoms
- Cough ( for at least 3 month a year for 2 consecutive years)
- Sputum (scantly mucoid or profuse mucopurulent or purulent)
- Breathlessness
- Similar attacks in past
- Restless
- Signs
- Respiratory rate = Increased
- Pulse rate = Increased and bounding
- Temperature = Raised or normal
- Blood Pressure = Normal or high or low
- General Examination
- Cynosis
- Polycythaemia due to presistent hypoxia(Hb>18 gm%)
- Feature of right heart failure
- Hepatomegaly
- Pedal oedema
- Flapping tremor (due to CO2 narcosis)
- Drowsy and retless ( due to hypoxia)
- Use of accessory muscles of respiratory
- Built is thin and weak
- Tracheal tug ( Trachea descend inspiration)
Chest examination
Inspection
- Prominent accessory muscles of respiration
- Hyper inflated chest,increased antero- posterior diameter of chest
- Indrawing of the costal margins and intercostal spaces.
- During inspiration we can find excavation of the suprasternal and supraclavicular fossae.
palpation
- Tracheal tug
- Decreased length of palpable trachea above sternal notch
- Diminished chest expansion
Percussion
- Hyperesonance of lung field
- Auscultation
- Vesicular breathing, sound with prolonged inspiration
- Rhonchi ( inspiratory and expiratory)
- Crepitations when there is associated chest infection
- Cardiac murmur ( tricuspid regurgitation: Pansystolic murmur in tricuspid area)
Investigations
- Chest x-ray PA views
Findings:
- Tubular heart
- Hyper inflated lung field of chronic obstructive pulmonary disease
- Low flat diaphragm
- Emphysematous bulla
- Pneunothorax ( complication)
- Association chest infection
(Hyperinflated:> 6anterior ribs seen above the diaphragm in mild- clavicular line)
- Blood:
- Hb% Increased
- ESR Increased
- TC,DC,(Leucocytosis)
- Sputum
- Gram stain
- Culture and sensitivity test(C/S)
- AFB staining
- Spirometry
- Reduced forced expired volume in 1 secound
- Reduced forced expired volume and vital capacity ratio(FEV1<80%FEV1/VC<70%)
- Increased Total Lung Capacity (TLC)
- Increased Residual Volume (RV)
- Arterial blood gas analysis
- Hypoxia and Hypercarbia( increase CO2)
- ECG
- Sinus tachycardia
- P- pulmonale ( height of P- wave more than 2.4mm in ledd II)
- Right ventriculat hypertrophy ie R- wave mor than S-wave in V1.
- Echocardiography
- Right atrium and right ventricle enlargement
- Tricuspid regurgitation
Drugs used in Management/ Treatment of chronic obstructive pulmonary disease (COPD)
Management/ Treatmentof COPD consist of
- Non-pharmacological Rx of COPD
- To prevent from cold,dust particles,and smoking.
- Avoid smoking of cigarrate
- Supplement of oxygen therapy
- Prevent from lings irritants such as air pollutions,
- Chemical fumes, or dust particals.
- Don't eat freeze substances
- To drink warm water with ginger or tulshi leaf.
- Pharmacological Rx of COPD
- Bronchodilators:
- Sympathomimetics : salbutamol,Terbutaline,Bambuterol,Salmeterol,Formoterol.
- Methylxantines(directly acting brochodilators): Theophylline, Aminophylline,Doxophylline.
- Anticholinergics( blocks action of acetylcholine (Ach )on autonomic effects):Ipratropium bromide,Tiotropium bromide.
- Leukotriene antagonist: Montelukast, Zafirlukast
- Corticosteroids:
- Systemic: Hydrocortisone, Prednisolone.
- Inhalational: Beclomethasone dipropionate,Budesonide, Fluticasone propionate,Flunisolide, Ciclesonide.
- Antibiotics:
- Macrolides eg: Azithromycine
- Penicillins eg: Amoxycillin,calvulanic acid,
- Cephalosporins.
- Cortimoxazole
- Mucolytics: Bromhexine,Ambroxol, Acetylcysteine,Carbocisteine.
- Morphine and Codeine : To reduce your coughing and to help with breathlessness in severe case .




0 Comments
If you have any question regarding this post, please let me know.